U.S. maternal mortality has reached alarmingly high levels, surpassing that of other high-income countries and highlighting critical issues within our maternal health care system. A recent study revealed that more than 80 percent of pregnancy-related deaths in the United States are preventable, yet the mortality rate continues to rise. Between 2018 and 2022, factors such as persistent disparities in maternal health and the impact of the COVID-19 pandemic contributed to this troubling trend. The statistics are particularly stark among racial and ethnic minorities, where women of color face overwhelming risks during and after pregnancy. Addressing the high maternal mortality rate requires urgent improvements in both prenatal and postpartum care, as well as comprehensive policies to ensure equitable health outcomes for all women.
The alarming rise in maternal deaths in the U.S. reflects deep-rooted issues within the healthcare framework, encompassing both pre- and postnatal care. This public health crisis can be characterized by the term “pregnancy-related fatalities,” which underscores the preventability of many of these deaths if adequate medical support is provided. Furthermore, understanding the rotational dynamics behind postpartum complications reveals a pressing need for systemic reform in maternal health services. Disparities in maternal wellness are evident, with clear racial inequalities that demand immediate attention and action from policymakers. In exploring the nuances of high maternal mortality, it becomes crucial to advocate for comprehensive strategies that bolster care standards and reduce the risk for all expectant mothers.
Understanding the High Maternal Mortality Rate in the U.S.
The United States has long been criticized for its perplexingly high maternal mortality rate, particularly compared to other high-income countries. More than 80% of the pregnancy-related deaths in the U.S. are preventable, indicating systemic issues rather than unavoidable medical complications. The disparities highlighted in recent studies point to the need for targeted interventions in maternal health care that address the unique challenges faced by different racial and ethnic groups. American Indian and Alaska Native women, for instance, are disproportionately affected, experiencing mortality rates that are nearly four times higher than their white counterparts.
Moreover, the healthcare infrastructure in the U.S. is often fragmented, leading to significant gaps in care. Issues such as maternity care deserts and lack of access to comprehensive prenatal and postpartum services create barriers for expectant mothers, particularly those from marginalized communities. The interplay between socioeconomic status, race, and geography suggests that a more equitable approach to maternal health is crucial in reversing these trends. Enhancing access to quality maternal health services can significantly reduce pregnancy-related deaths, thereby improving outcomes for women across the nation.
The Importance of Extended Postpartum Care
Extended postpartum care is often overlooked in the conversation about maternal health, yet it plays a critical role in reducing the incidence of pregnancy-related deaths. Recent research shows that nearly a third of maternal deaths occur from complications that arise between 42 days to a year postpartum. Traditionally, the healthcare system has set a cutoff at six weeks after childbirth, creating a dangerous gap in care where many women are left without necessary support. By recognizing that postpartum recovery is a continuum rather than a finite period, healthcare providers can better address the needs of mothers during this crucial time.
Improving postpartum care requires a systemic overhaul of how healthcare services are delivered. Programs should be designed to provide ongoing support beyond the initial postpartum visit, including mental health screenings and management of chronic conditions like hypertension or cardiovascular diseases that have become leading causes of maternal mortality. By investing in comprehensive extended postpartum care, healthcare systems can ensure better health outcomes for mothers and their children, ultimately addressing the disparities that have persisted across different demographics.
Disparities in Maternal Health and Racial Equity
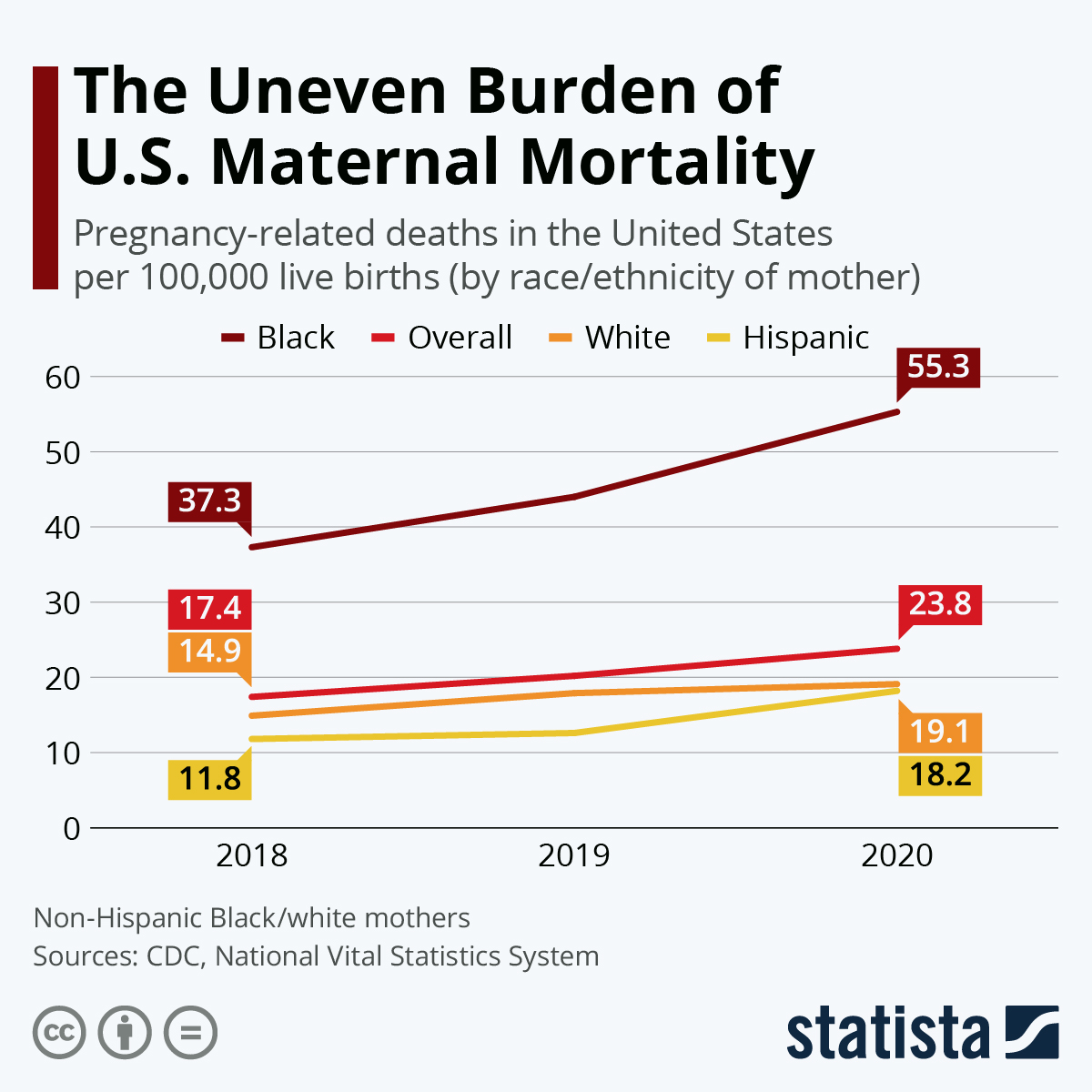
The pronounced disparities in maternal health outcomes across racial and ethnic lines in the U.S. highlight a pressing need for targeted interventions and policy changes. Research indicates that non-Hispanic Black women and American Indian women are far more likely to experience pregnancy-related deaths than their white counterparts. These disparities are rooted in a combination of factors, including systemic racism, variations in healthcare access, and differences in the quality of care received. Addressing these inequities requires a comprehensive strategy that includes anti-racist training for healthcare providers and community outreach programs to educate and empower at-risk populations.
Policy initiatives aimed at reducing these disparities can be highly effective if implemented correctly. For instance, expanding Medicaid eligibility and coverage for maternal health services can significantly increase access to care for low-income women. Furthermore, establishing community health worker programs can bridge the gap between healthcare systems and underserved populations, ensuring that all women receive the support they need throughout their pregnancies. By prioritizing racial equity in maternal health discourse, we can work towards a more just healthcare system that meets the needs of every mother.
Enhancing Maternal Health Care Systems in the U.S.
To combat the rising trend of maternal mortality, it is imperative to rethink and enhance the existing maternal health care systems in the U.S. The current healthcare landscape is often fragmented, exacerbating the challenges that pregnant individuals face when seeking care. To combat this, a more integrated approach is necessary, one that provides continuous, high-quality care throughout pregnancy and beyond. Investments in public health infrastructure are vital for tracking maternal deaths accurately and implementing effective interventions that mitigate risks.
Emphasizing quality improvement initiatives within healthcare systems can also lead to better outcomes for mothers. By adopting evidence-based practices and fostering an environment of accountability, maternal health care providers can address the complex needs of their patients while ensuring that disparities are tackled head-on. As recent studies suggest, states that have implemented comprehensive maternal health programs have witnessed notable decreases in pregnancy-related deaths. This serves as a blueprint for other states aiming to enhance maternal health care and decrease mortality rates.
Preventable Causes of Maternal Mortality
It’s alarming that a significant majority of pregnancy-related deaths in the U.S. are deemed preventable, pointing to flaws in the maternal health care system. Conditions like cardiovascular disease have emerged as leading causes of maternal deaths, overshadowing complications like hemorrhage that previously held that title. This transition highlights the need for better management and awareness of chronic conditions among expectant mothers. Health professionals must prioritize screening and managing such conditions to prevent deaths that can be avoided with proper care.
Education around recognizing early warning signs of potential complications during pregnancy and postpartum can empower mothers to seek help proactively. Collaborative efforts involving maternal health providers, public health officials, and community organizations can facilitate a more robust response to preventable causes of deaths. By integrating educational programs and accessible healthcare resources, we can create an environment where expectant mothers have the knowledge and support they need to navigate their health journeys safely.
Cardiovascular Health and Maternal Mortality
Recent findings reveal that cardiovascular health is emerging as a significant concern within the context of maternal mortality. With approximately 20% of pregnancy-related deaths attributed to cardiovascular issues such as hypertension and heart disease, this trend indicates that the typical ages for these conditions are shifting. A growing number of women experience conditions like chronic hypertension earlier in life, which elevates their risk during pregnancy and postpartum.
Addressing cardiovascular health within the maternal care framework is essential for improving outcomes. Health providers must actively manage and monitor the cardiovascular status of pregnant individuals, especially those with pre-existing conditions, to mitigate the risk of severe complications. Furthermore, raising awareness about the importance of heart health among women of reproductive age can build resilience against these life-threatening challenges during and after pregnancy.
The Role of Hospital Systems in Maternal Health
Hospital systems play a pivotal role in determining maternal health outcomes, yet there is much room for improvement in the care provided. Many hospitals lack adequately equipped maternity units capable of dealing with complications, which often leads to inadequate management of high-risk pregnancies. Facilities must adopt best practices and evidence-based protocols to ensure safe delivery experiences for mothers. This can mean expanded training for obstetric staff to recognize and respond effectively to complications, enhancing the quality of care provided.
Additionally, creating partnerships between hospitals and community organizations can foster a more supportive environment for expectant mothers. By providing seamless transitions from prenatal care to delivery and postpartum follow-up, hospitals can help bridge gaps that often result in negative health outcomes. Furthermore, developing clear communication strategies among healthcare providers, patients, and families will ensure that maternal health is prioritized, safeguarding the health and well-being of mothers in their care.
Investing in Public Health Infrastructure for Maternal Health
The current state of maternal health in the U.S. underscores a critical need for robust investment in public health infrastructure. This is particularly urgent given that the rates of pregnancy-related deaths have dramatically increased over recent years, indicating that the status quo is not acceptable. Enhancing public health resources dedicated to maternal health not only focuses on tracking maternal deaths accurately but also helps inform policy changes that can enhance healthcare delivery systems across the nation.
Investment should also focus on prevention programs that educate women about maternal health risks and encourage access to prenatal and postpartum care. Comprehensive initiatives that include training for healthcare providers on cultural competencies and managing health disparities can lead to better outcomes for marginalized groups disproportionately affected by high maternal mortality rates. Furthermore, stakeholders must prioritize maternal health on the national agenda to ensure that both financial and policy commitments are aligned with the pressing needs of pregnant individuals in the U.S.
Addressing Late Maternal Deaths and Postpartum Care
The growing recognition of late maternal deaths—those occurring more than 42 days postpartum—highlights a critical area of concern in maternal health. The fact that these deaths account for nearly a third of maternal mortality cases emphasizes the need for extending care beyond the immediate postpartum period. Many healthcare systems operate under the assumption that care is no longer needed after six weeks; however, this perspective neglects the ongoing physical and mental health challenges that new mothers can face.
Creating a healthcare model that includes comprehensive postpartum support is essential for addressing these late maternal deaths. This should involve regular health screenings, mental health resources, and support for chronic conditions that may develop or worsen during pregnancy. Furthermore, engaging with mothers through community support networks can strengthen their health outcomes and reduce the incidence of preventable deaths. By recognizing the postpartum period as a critical phase of maternal health, stakeholders can usher in necessary changes to improve care and support.
Frequently Asked Questions
What are the main causes of U.S. maternal mortality?
The main causes of U.S. maternal mortality include cardiovascular disease, hemorrhage, and hypertensive disorders, with cardiovascular disease accounting for over 20% of pregnancy-related deaths. The rising prevalence of chronic conditions among women of reproductive age contributes significantly to the high maternal mortality rate in the U.S.
Why does the U.S. have a high maternal mortality rate compared to other high-income countries?
The U.S. has a high maternal mortality rate due to various factors, including a fragmented healthcare system, inequitable policies, and the presence of maternity care deserts. Additionally, persistent biases and discrimination across racial and ethnic groups exacerbate disparities in maternal health.
How do racial disparities impact maternal health outcomes in the U.S.?
Racial disparities significantly impact maternal health outcomes, with American Indian and Alaska Native women experiencing the highest maternal mortality rates, followed by non-Hispanic Black women. These disparities are indicative of larger systemic issues within the healthcare system that necessitate urgent policy changes.
What role does postpartum care play in reducing maternal mortality in the U.S.?
Postpartum care is crucial in reducing maternal mortality, as nearly a third of pregnancy-related deaths occur during the postpartum period. Expanding healthcare services beyond the initial six weeks postpartum can improve outcomes and address the continuum of care needed by new mothers.
What innovative solutions are needed to address U.S. maternal mortality?
To address U.S. maternal mortality, innovative solutions must focus on improving the quality of maternity care, increasing access to healthcare services during both pregnancy and the extended postpartum period, and implementing equitable policy changes across states.
How can the U.S. reduce preventable pregnancy-related deaths?
The U.S. can reduce preventable pregnancy-related deaths by enhancing public health infrastructure, ensuring better access to quality prenatal and postpartum care, addressing chronic health issues in reproductive-age individuals, and focusing on reducing disparities based on race and socioeconomic status.
What impact did the COVID-19 pandemic have on maternal mortality rates in the U.S.?
The COVID-19 pandemic significantly impacted maternal mortality rates in the U.S., with a notable increase in pregnancy-related deaths recorded in 2021. The pandemic underscored existing weaknesses in the healthcare system, highlighting the need for improved maternal healthcare policies and support.
Why is tracking maternal deaths important for improving maternal health care?
Tracking maternal deaths is vital for improving maternal health care as it provides essential data that can inform policy decisions, identify systemic issues, and guide investments in healthcare infrastructure. Accurate tracking allows for targeted interventions that can reduce preventable maternal deaths.
What should be prioritized in U.S. maternal health policy moving forward?
Moving forward, U.S. maternal health policy should prioritize investments in public health infrastructure, equitable access to quality prenatal and postpartum care, and strategies to address the underlying causes of racial and ethnic disparities in maternal mortality.
| Key Points | Details |
|---|---|
| U.S. Maternal Mortality Rate | The U.S. has the highest maternal mortality rate among high-income countries, which rose from 25.3 deaths per 100,000 live births in 2018 to 32.6 in 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths are preventable. |
| Disparities by Race | American Indian and Alaska Native women had the highest mortality rate at 106.3 deaths per 100,000 live births, while White women had the lowest at 27.6. |
| COVID-19 Impact | The sharpest increase in mortality rates occurred in 2021, likely due to the pandemic. |
| Leading Cause of Death | Cardiovascular disease is the leading cause, accounting for over 20% of deaths. |
| Policy Recommendations | Investment in public health infrastructure and innovative solutions is necessary to improve maternal health outcomes. |
Summary
U.S. maternal mortality is a pressing concern that emphasizes the need for systemic changes in healthcare. With the nation leading high-income peers in maternal mortality rates and witnessing ongoing increases, particularly among vulnerable populations, it is vital to implement better prenatal and extended postpartum care. Strategies must focus on reducing avoidable deaths and addressing the significant disparities that affect racial and ethnic groups within the healthcare system. A cooperative effort to enhance public health infrastructure and policy initiatives is essential in reversing these alarming trends.