TIM-3 Alzheimer’s treatment represents a significant breakthrough in the realm of Alzheimer’s disease research, leveraging the body’s immune system to combat plaque accumulation in the brain. Recent studies have demonstrated that by targeting the TIM-3 molecule, scientists can enhance the activity of brain immune cells known as microglia, enabling them to effectively clear harmful plaques associated with Alzheimer’s. This innovative approach not only improves cognitive function but also holds promise for future therapeutic strategies in managing this debilitating condition. As researchers delve deeper into the relationship between TIM-3 and Alzheimer’s, the implications for immune system therapy in neurological contexts continue to expand. Understanding how the TIM-3 molecule interacts with microglia may lead to transformative treatments aimed at restoring memory and cognitive abilities in affected individuals.
Exploring the TIM-3 pathway offers a new lens on treating Alzheimer’s disease, a neurodegenerative condition characterized by the accumulation of amyloid plaques. By focusing on the immune responses within the brain, specifically through checkpoint molecules like TIM-3, researchers aim to unlock potential therapies that could radically alter the disease’s progression. This method harnesses the brain’s own immune mechanisms, namely microglial cells, to tackle the underlying issues of plaque buildup. The promotion of cognitive enhancement through TIM-3 modulation could revolutionize current strategies in Alzheimer’s care. Overall, this emerging field highlights a fascinating intersection of neural health and immune function, indicating a collaborative approach may yield optimal results in cognitive function improvement.
Understanding TIM-3 and Its Role in Alzheimer’s Disease
TIM-3, or T cell immunoglobulin and mucin domain-containing protein 3, is a significant molecule in the landscape of immunology, particularly concerning Alzheimer’s disease research. This checkpoint molecule, identified as an inhibitory factor, plays a crucial role in regulating microglial activity in the brain. In Alzheimer’s patients, an increased expression of TIM-3 on microglia correlates with the inability of these immune cells to effectively clear amyloid beta plaques, a characteristic feature of the disease. This impaired function of microglia can significantly compromise cognitive function, making understanding TIM-3’s role imperative for developing future therapies.
Studies have shown that by deleting the TIM-3 gene in mouse models, researchers can improve the cognitive behaviors associated with Alzheimer’s. Mice without TIM-3 exhibited less plaque buildup and demonstrated enhanced memory capabilities. This has prompted scientists to explore therapeutic avenues targeting TIM-3, aiming to create treatments that could potentially modulate its expression. Such strategies could pave the way for innovative immune system therapies, not only for Alzheimer’s but possibly for other neurodegenerative conditions where plaque build-up is a concern.
The Impact of Immune System Checkpoint Molecules
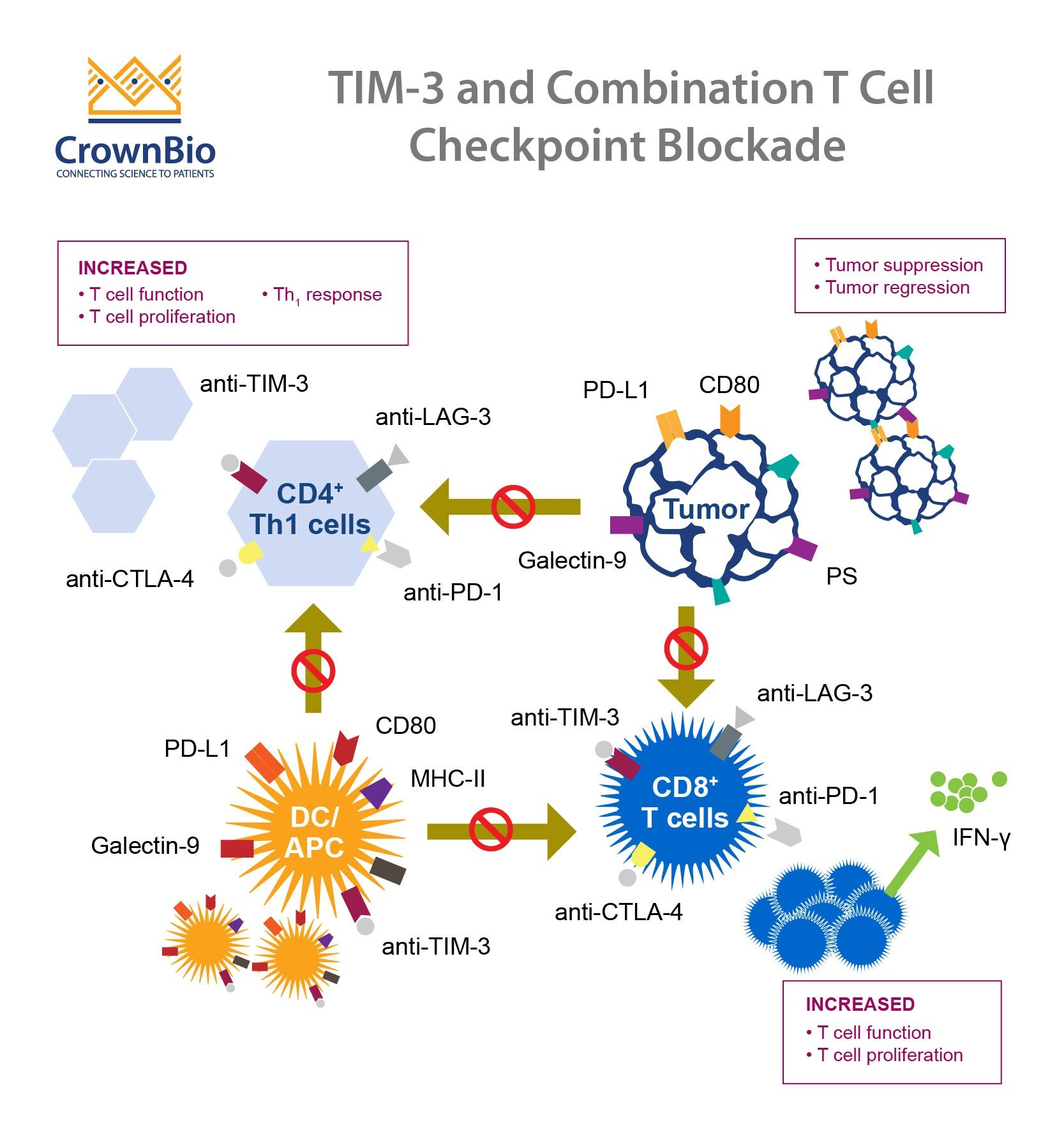
Checkpoint molecules have been a focal point in cancer immunotherapy, and their role in neurological disorders is garnering increasing attention. In the context of Alzheimer’s disease, the TIM-3 molecule serves as a brake on the immune system, preventing microglia from engaging in their protective functions. When the immune cells are restrained, dangerous plaques accumulate in the brain. This situation hints at a novel approach wherein inhibiting TIM-3 could potentially unleash the microglia, enabling them to clear out amyloid plaques and restore some degree of cognitive function, an exciting prospect for patients suffering from Alzheimer’s.
Recent findings suggest that targeting such molecules could fundamentally change how we approach Alzheimer’s disease treatment. By designing therapies that either block the action of TIM-3 or reduce its expression selectively in individuals with Alzheimer’s, researchers hope to restore the immune system’s ability to clear debris and plaques from the brain. These developments underscore the promising intersection of cancer and Alzheimer’s research, where insights into immune system therapies could lead to breakthroughs in combating this devastating disease.
Microglia, TIM-3, and Cognitive Function Improvement
Microglia are the brain’s resident immune cells, vital for maintaining homeostasis and responding to pathological changes. In normal function, they prune unnecessary synapses during development; however, in aging and Alzheimer’s, microglial activation leads to problematic outcomes, particularly due to the elevated presence of TIM-3. The excessive expression of TIM-3 hinders the microglia’s ability to engulf amyloid beta plaques. This results in cognitive decline, as the accumulation of plaques correlates with memory impairment and other cognitive dysfunctions observed in Alzheimer’s patients.
Studies have indicated that by inhibiting TIM-3, the microglial response can be restored, allowing these cells to actively remove harmful plaques from the brain. Animal models demonstrating improved cognitive function after TIM-3 inhibition highlight an essential breakthrough in Alzheimer’s treatment strategies. This research lays a foundation for developing specific TIM-3 therapies that could be used alongside established treatment regimens, aiming for enhanced overall cognitive function and quality of life for those living with Alzheimer’s.
The Future of TIM-3 Therapy in Alzheimer’s Treatment
As we look ahead, the potential for TIM-3 inhibitors to revolutionize Alzheimer’s treatment appears promising. With existing anti-TIM-3 antibodies already being used in cancer therapies, researchers are exploring their repurposing for Alzheimer’s disease. These antibodies can potentially facilitate the activation of microglia, enhancing their ability to clear toxic plaques while also improving cognitive function. The challenge lies in ensuring that these treatments can selectively target brain cells without causing unwanted side effects elsewhere in the body.
Moreover, ongoing research aims to assess the efficiency of human anti-TIM-3 antibodies in mouse models that closely mimic the human Alzheimer’s disease phenotype. Successful outcomes could fast-track clinical trials, ultimately leading to novel therapies that can transform how we combat Alzheimer’s. The successful application of TIM-3 therapies would not only signify a breakthrough for Alzheimer’s patients but could also reshape the entire field of neurodegenerative disorder treatment, enhancing our understanding of immune modulation in the brain.
Insights into Amyloid Plaque Clearance via TIM-3 Manipulation
Research has unveiled that amyloid plaques, a trademark of Alzheimer’s disease, can be targeted by manipulating the TIM-3 signaling pathway. As microglia exhibit heightened expression of TIM-3 when activated, this prevents them from clearing amyloid beta deposits effectively. This novel angle in Alzheimer’s disease research encourages a reconsideration of traditional therapeutic strategies, suggesting that enhancing the immune response through TIM-3 inhibition may allow microglia to regain their ability to manage plaque accumulation and restore brain function.
By focusing on the mechanisms surrounding TIM-3, scientists could re-engineer therapies that make use of the body’s own immune defenses. Adopting such an approach not only highlights the potential for improved cognitive outcomes but also necessitates further investigation into how TIM-3 affects various brain functions in Alzheimer’s patients. This could lead to the development of more nuanced therapies that adaptively modulate microglial activity in response to different stages of Alzheimer’s pathology.
Microglial Dysregulation: The TIM-3 Interaction in Alzheimer’s
Dysregulation of microglial activity through overexpression of TIM-3 underscores the complexity of immune dysfunction in Alzheimer’s disease. These immune cells, while critical in maintaining brain health, become counterproductive in the face of accumulating amyloid plaques. The physical evidence shows that microglia, bound by insufficient activation due to TIM-3, fail to perform the essential task of clearing harmful substances, resulting in neuroinflammation and cognitive decline. This directly links TIM-3’s activity to the progression of Alzheimer’s disease.
Consequently, targeting TIM-3 not only has the potential to reactivate microglia but also aims to restore balance to immune responses in the brain. Addressing this dysregulation presents a profound opportunity to develop innovative treatments that harness natural immune mechanisms for therapeutic effect. With ongoing research focused on elucidating TIM-3’s precise role, we stand to gain crucial insights that could significantly alter treatment paradigms for Alzheimer’s and possibly other neurodegenerative disorders.
Exploring Genetic Factors in TIM-3 Expression and Alzheimer’s
Genetic factors significantly influence the expression of TIM-3 and its subsequent impact on Alzheimer’s disease. For instance, variations in the HAVCR2 gene associated with TIM-3 have been identified as risk factors for developing late-onset Alzheimer’s. Individuals with certain polymorphisms of this gene display heightened levels of TIM-3 expression on microglia, linking genetic predisposition directly with immune responses and disease pathology. Such insights underscore the importance of integrating genetic research within Alzheimer’s studies.
By exploring genetic contributions to TIM-3 expression, researchers can target therapeutic approaches based on individual genetic profiles. This precision medicine model could enable tailored interventions that enhance the efficacy of TIM-3 inhibitors, providing personalized care that considers a patient’s unique genetic makeup. Advancements in understanding these genetic predictors not only facilitate targeted therapies but also enrich the overall framework of Alzheimer’s research, revealing new avenues for treatment strategies.
Challenges and Opportunities in Treating Alzheimer’s with TIM-3 Antibodies
Despite the promising potential of TIM-3 antibodies for treating Alzheimer’s disease, several challenges remain. One significant concern is ensuring the selectivity of these antibodies designed to target and modulate TIM-3’s effects without causing unintended immune responses elsewhere in the body. As seen in previous trials, broad-spectrum approaches can lead to adverse outcomes, emphasizing the need for precision in targeting the specific immune pathways involved in Alzheimer’s pathology.
Nevertheless, these challenges present great opportunities for further research and development. Tailoring TIM-3 therapies to optimize their therapeutic window may yield significant advancements in alleviating the cognitive decline associated with Alzheimer’s. Collaborative efforts in the scientific community to explore optimal delivery methods, dosing regimens, and combination therapies could dramatically enhance the efficacy of TIM-3 focused treatments and improve the life quality of those afflicted by this condition.
The Role of Research Collaboration in Advancing TIM-3 Therapies
Collaboration among researchers is essential in advancing our understanding and application of TIM-3 therapies for Alzheimer’s disease. The synthesis of interdisciplinary knowledge from neurology, immunology, and genetics enables more robust experimental designs and data interpretation. By working collectively, scientists can share insights, resources, and methodologies, which accelerates the pace of discovery and refines therapeutic targets.
This collaborative effort is exemplified by ongoing projects where institutions pool their expertise to investigate the multifaceted roles of TIM-3 in Alzheimer’s. Encouraging synergy among research teams not only elevates the quality of investigations but also strengthens the overall impact of findings on future clinical practices. As we aim for meaningful breakthroughs, fostering collaboration will be pivotal in realizing the full potential of TIM-3 as an innovative therapeutic target.
Frequently Asked Questions
What is TIM-3 in relation to Alzheimer’s treatment?
TIM-3 is an immune checkpoint molecule that has been identified as a significant factor in Alzheimer’s disease. Research indicates that by inhibiting TIM-3, we can enhance the ability of microglia, the brain’s immune cells, to clear amyloid plaques, which may improve cognitive function in Alzheimer’s patients.
How does TIM-3 affect microglia in Alzheimer’s disease?
In Alzheimer’s disease, the expression of TIM-3 on microglia prevents them from attacking harmful amyloid plaques. This inhibition impairs the immune response, leading to plaque accumulation and cognitive decline. Targeting TIM-3 could enable microglia to resume their function in clearing these plaques.
What results have studies shown concerning TIM-3 and cognitive function improvement?
Studies involving genetically modified mice lacking the TIM-3 molecule have demonstrated improved clearance of amyloid plaques and subsequent enhancements in cognitive behavior. These findings suggest that TIM-3 therapies could lead to significant improvements in cognition for Alzheimer’s disease.
Can TIM-3 therapies be applied to human Alzheimer’s treatment?
Yes, TIM-3 therapies, potentially utilizing anti-TIM-3 antibodies or small molecules that inhibit TIM-3 action, are being explored for human applications. This novel approach aims to enhance microglial activity in clearing plaques, thereby addressing a core mechanism of Alzheimer’s pathology.
What is the significance of TIM-3 gene polymorphism in Alzheimer’s disease patients?
In Alzheimer’s disease patients, a polymorphism in the TIM-3 gene (HAVCR2) is associated with higher levels of TIM-3 expression on microglia. This elevated expression prevents effective plaque clearance and is linked to the disease’s progression, highlighting TIM-3’s role as a therapeutic target.
How does the immune system’s role in Alzheimer’s relate to cancer treatment strategies?
The immune system strategies that have been successful in cancer treatment, particularly those targeting checkpoint molecules like TIM-3, may also be applicable in Alzheimer’s disease. By reactivating microglial responses, therapies that inhibit TIM-3 could restore cognitive functions affected by plaque accumulation.
What advancements have been made in TIM-3 research for Alzheimer’s disease?
Recent studies have shown that inhibiting TIM-3 can significantly improve plaque clearance by microglia and enhance cognitive functions in mouse models of Alzheimer’s. This research fosters hope for developing TIM-3-based therapies that could offer new treatment pathways for Alzheimer’s patients.
What are the challenges with existing Alzheimer’s treatments and how can TIM-3 provide a solution?
Current Alzheimer’s treatments often target amyloid beta directly, which can lead to vascular complications. TIM-3 offers a new avenue by potentially enabling microglia to clear plaques more effectively without the associated risks, making it a promising target for future research and therapy.
| Key Point | Details |
|---|---|
| Research Background | Study published in *Nature* focuses on TIM-3 and its role in Alzheimer’s. |
| Role of TIM-3 | TIM-3 inhibits microglia from clearing amyloid plaques in Alzheimer’s. |
| Microglial Function | Microglia are the brain’s immune cells that prune synapses and clear debris. |
| Polymorphism and Alzheimer’s | Alzheimer’s patients with a specific TIM-3 gene polymorphism exhibit higher TIM-3 expression. |
| Research Findings | Deletion of TIM-3 in lab mice improves memory and plaque clearance. |
| Therapeutic Implications | Potential development of TIM-3 inhibitor therapy to treat Alzheimer’s. |
| Future Research | Testing human anti-TIM-3 antibodies to prevent plaque development in Alzheimer’s mouse models. |
Summary
TIM-3 Alzheimer’s treatment represents a promising avenue in Alzheimer’s disease research. By targeting the TIM-3 molecule, researchers aim to enhance the immune response of microglia to effectively clear amyloid plaques from the brain, potentially restoring memory function and cognitive abilities. This innovative approach may lead to breakthrough therapies for the millions affected by Alzheimer’s, particularly those suffering from late-onset forms of the disease. Continued exploration into TIM-3 mechanisms and targeted therapies is essential to advance our understanding and treatment of Alzheimer’s disease.