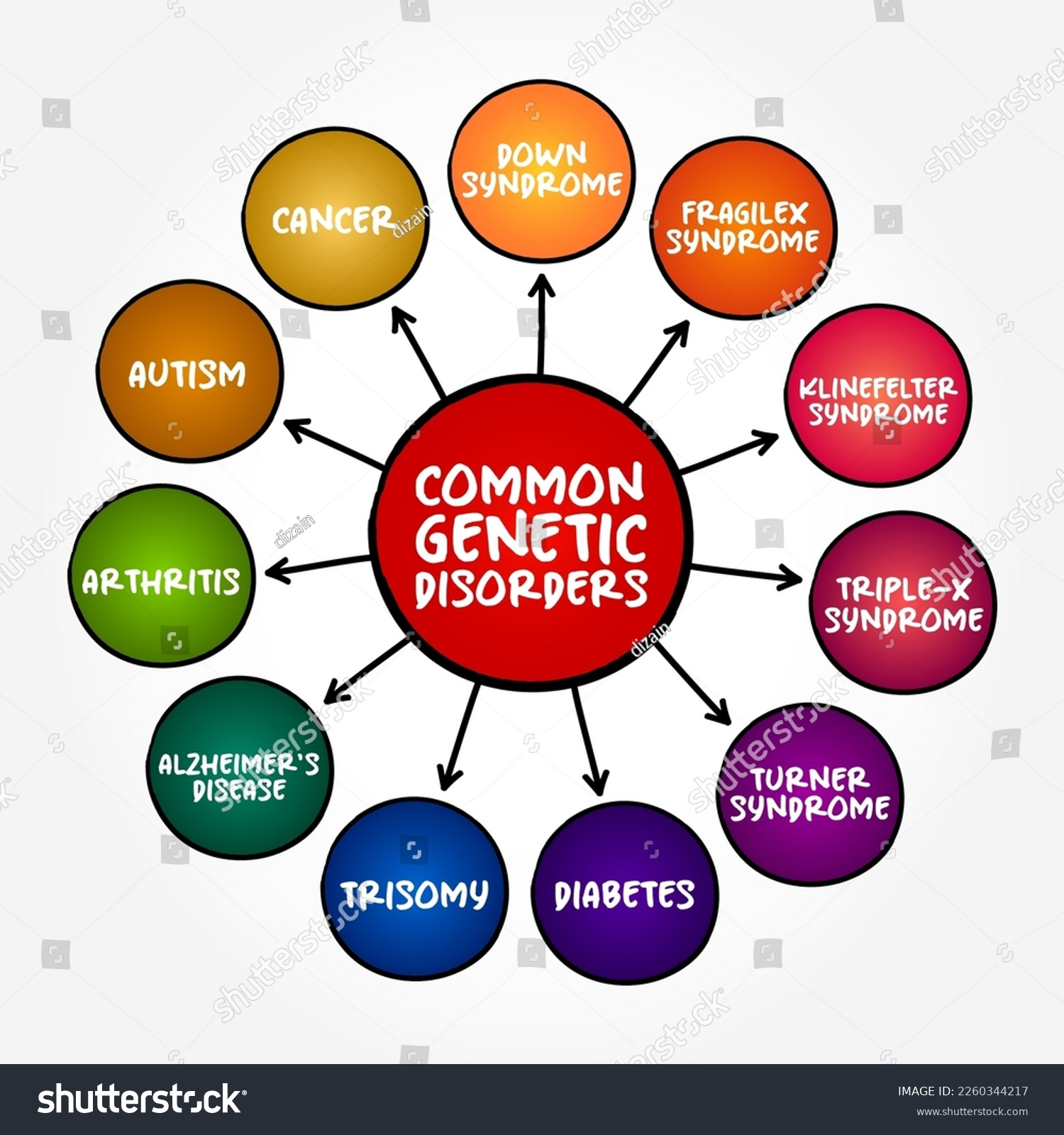
Genetic disorders pose significant challenges to families and healthcare providers alike, particularly during the delicate stages of pregnancy. Recent advancements in prenatal genetic testing have opened new horizons for detecting these conditions before birth, allowing for timely interventions that can drastically improve outcomes. A groundbreaking study has identified nearly 300 genetic disorders that are treatable, forming a vital “treatable fetal conditions” list that could revolutionize prenatal care. Through early intervention in pregnancy, expectant parents can learn about possible genetic disorders treatment options and engage in fetal therapy that may prevent severe consequences for the newborn. As we explore the evolving landscape of genetic diagnostics, understanding these disorders becomes crucial in fostering healthier futures for children and their families.
When discussing hereditary conditions, the term “genetic disorders” encompasses a wide array of issues linked to chromosome and gene abnormalities. These hereditary health conditions can manifest in various ways and often require specialized care and management strategies. Innovations in prenatal screening methods have made it possible for healthcare providers and families to identify treatable fetal conditions early on, paving the way for tailored interventions. By emphasizing the importance of early detection and management, attention to these disorders is helping to shape a future where proactive prenatal care becomes the norm. These advancements are integral in ensuring that families are equipped to handle the implications of genetic predispositions.
Introduction to Treatable Fetal Conditions
Medical advancements have increasingly highlighted the importance of identifying treatable fetal conditions before birth. Recent studies have shed light on nearly 300 genetic disorders that can potentially be addressed during pregnancy, leading to better outcomes for both fetuses and newborns. This breakthrough comes through the innovative application of prenatal genetic testing techniques that can pinpoint conditions early in the gestation period, providing an invaluable opportunity for intervention.
By developing a comprehensive list of treatable fetal findings, healthcare professionals can guide expectant parents through the complexities of prenatal care. Early intervention in cases of identified conditions not only increases the chances of successful treatment but also significantly reduces the morbidity associated with many genetic disorders. This proactive approach signifies a transformative shift in our capabilities to manage fetal health.
The Role of Prenatal Genetic Testing
Prenatal genetic testing plays a pivotal role in early detection of genetic disorders. With advancements in genomic sequencing, healthcare providers can detect underlying genetic conditions before birth. Such diagnostics serve not only to inform parents but also to allow medical teams to prepare for potential interventions needed immediately post-delivery. The information obtained from these tests can help navigate the complexities of fetal therapy and guide families toward informed decisions regarding treatment options.
This process can demystify the fears surrounding genetic disorders by providing clear pathways to care. The diagnostic information allows for targeted strategies to mitigate risks associated with certain conditions, empowering parents through critical early interventions. Furthermore, it paves the way for comprehensive planning by obstetricians and geneticists working together to ensure optimal outcomes.
Advancements in Genetic Disorders Treatment
The treatment of genetic disorders has seen remarkable improvements over the past decade, largely due to advancements in fetal therapy. With the identification of genetic disorders that are actionable during pregnancy, doctors can offer tailored solutions that cater to the specific needs of each unborn child. For instance, conditions that affect cardiovascular or gastrointestinal systems can sometimes be managed prenatally, leading to a significant reduction in complications at birth.
This shift towards a more proactive treatment paradigm means that families now have the option to address and potentially alter the course of their child’s health from before birth. Researchers underscore the importance of timely intervention, affirming that early diagnosis can meaningfully change outcomes, reducing long-term health burdens associated with many genetic disorders.
Ethical Considerations in Genetic Testing
As beneficial as the advancements in prenatal genetic testing may be, they also come with a range of ethical considerations. The decision to undergo genetic screening can be overwhelming for expectant parents, who may face anxiety related to potential outcomes. Physicians and genetic counselors must navigate these conversations delicately, ensuring that families feel supported throughout the decision-making process.
The role of ethics in the context of early intervention is crucial, especially as healthcare teams strive to balance providing information against the emotional weight it carries. By engaging ethicists alongside medical professionals, there is a greater opportunity to develop best practices that prioritize patient autonomy while also offering the necessary guidance through complex medical information.
Enhanced Collaboration for Improved Care
Creating a targeted list of treatable fetal conditions mandates a collaborative approach among healthcare professionals. Obstetricians, geneticists, and ethicists must work cohesively to ensure that patients receive clear and comprehensible information about prenatal genetic testing and treatment options. This teamwork is essential for ensuring that families are presented with opportunities for early intervention that may change the trajectory of genetic disorders.
Moreover, such collaborations foster an environment where medical professionals can address concerns, clarify misconceptions, and ultimately enhance patient experience. By aligning clinical aims with patient needs, healthcare teams can significantly improve care outcomes and lay a foundation for positive health trajectories.
The Impact of Early Intervention in Pregnancy
Early intervention in pregnancy has shown to positively impact the health and well-being of both the fetus and the family unit. By identifying treatable fetal conditions early, families can avoid dire outcomes associated with delayed treatment. For instance, disorders indicative of serious health risks can be managed through careful monitoring and medical interventions, allowing children to thrive from the onset.
The data suggests that when timely interventions are employed, it not only reduces morbidity rates but also minimizes the emotional and financial burdens typically associated with prolonged treatment regimens postnatally. This foresight allows parents to prepare both emotionally and logistically for their child’s health journey, transforming uncertainty into clear actions and strategies.
The Future of Fetal Medicine
The future of fetal medicine appears promising, with ongoing research and technological advancements playing pivotal roles. Initiatives aimed at expanding the treatable fetal findings list suggest that healthcare will continue to evolve, creating new avenues for managing genetic disorders in utero. This progressive outlook indicates that even more conditions may soon become treatable, ultimately enhancing the quality of care for expectant families.
As researchers continue to explore the genetic basis for a wide range of conditions, the hope is that innovative prenatal therapies will not only prevent complications but also allow for healthier outcomes from the very beginning of life. This evolution in fetal medicine emphasizes the importance of continued investment and collaboration within the medical community.
Family Support Systems During Pregnancy
Support systems are crucial for families navigating the complexities of genetic disorders that may be identified during pregnancy. The emotional aspects of learning about potential health issues can be daunting; thus, having a strong network of support is essential for expectant parents. Family, friends, and professional counseling all play vital roles in helping parents make informed decisions regarding genetic testing and intervention options.
Furthermore, organizations and support groups focused on genetic disorders can assist families in finding the resources they need to cope with the challenges associated with prenatal diagnoses. This communal approach can empower families, soothing the emotional turbulence that may accompany dire news while fostering a sense of solidarity in addressing future health concerns.
Navigating Postnatal Patient Care
The transition to postnatal care is an integral part of managing genetic disorders in newborns, especially when prenatal conditions have been diagnosed. Effective communication between prenatal and postnatal care teams is essential in ensuring that children receive timely treatment and interventions tailored to their specific needs from the moment they are born.
This seamless integration of care can significantly alter the health trajectory for newborns, paving the way for more comprehensive management strategies in dealing with identified genetic disorders. It strengthens the continuum of care, ensuring families have access to necessary therapies and supports right from birth, minimizing the impact of potential complications.
The Importance of Research Funding
Research funding is a vital pillar supporting advancements in prenatal genetic testing and treatment strategies. As highlighted in the recent study, initiatives backed by the National Institutes of Health and other funding bodies are essential to drive innovative research that could identify even more treatable fetal conditions. This financial investment facilitates exploration into new technologies, methodologies, and training opportunities for healthcare professionals.
With ongoing funding, researchers can continue to develop resources that empower families facing genetic disorders, leveraging the latest science to transform fetal care. By establishing robust research programs, we ensure that the future of prenatal care remains focused on improving health outcomes and providing actionable solutions for families and their children.
Frequently Asked Questions
What are treatable fetal conditions in relation to genetic disorders?
Treatable fetal conditions are specific genetic disorders identified during pregnancy that can be managed or treated either in utero or shortly after birth. A recent study outlined nearly 300 genetic disorders that fall into this category, emphasizing the potential for early intervention to improve outcomes.
How can prenatal genetic testing help in diagnosing genetic disorders?
Prenatal genetic testing, such as genomic sequencing, plays a crucial role in diagnosing genetic disorders by revealing abnormalities that may indicate treatable conditions. By identifying these disorders early, healthcare providers can offer timely interventions and treatment options to improve the health of the fetus.
What is the significance of early intervention in pregnancy for genetic disorders?
Early intervention in pregnancy is vital for genetic disorders because it allows for timely medical management of conditions that can be treated before birth or in the neonatal period. Research shows that addressing these disorders early can significantly reduce morbidity and improve long-term health outcomes for affected infants.
What options are available for genetic disorders treatment identified before birth?
Treatment options for genetic disorders identified before birth can include various fetal therapies, such as in utero surgeries or medication management, depending on the specific condition. These treatments aim to address the disorder proactively and enhance the baby’s health before and after delivery.
How do fetal therapies work in treating genetic disorders identified during pregnancy?
Fetal therapies involve medical interventions provided to the fetus while still in the womb, aiming to treat genetic disorders or mitigate their effects. These therapies can range from minimally invasive procedures to complex surgeries, and they are designed to improve the prognosis for conditions that, if untreated, could lead to severe complications after birth.
What challenges exist in managing genetic disorders during pregnancy?
While advancements in prenatal care have improved diagnosis and treatment of genetic disorders, challenges include ethical considerations regarding information overload for patients, the emotional burden of decision-making, and the need for comprehensive care teams to guide families through complex health information.
What role does genomic sequencing play in the detection of genetic disorders?
Genomic sequencing is a powerful tool in prenatal care, enabling the identification of genetic disorders by analyzing fetal DNA. This technology can uncover not only known conditions but also incidental findings that might indicate treatable disorders, allowing for timely interventions that can improve health outcomes.
| Key Points |
|---|
| Researchers identified nearly 300 genetic disorders treatable during pregnancy or shortly after birth. |
| The study aims to improve diagnosis and enhance treatment options for these conditions. |
| Genomic sequencing is crucial for prenatal diagnosis, informing potential interventions early. |
| Timely detection could significantly reduce morbidity and mortality for affected infants. |
| Ethical considerations and information overload for patients are potential challenges to this initiative. |
| Collaboration among healthcare professionals is vital to support families during this process. |
Summary
Genetic disorders represent a vital aspect of prenatal health that can now be addressed and treated before birth. Recent advancements in research highlight the possibility of identifying and managing nearly 300 genetic conditions during pregnancy, offering families a chance for proactive intervention. Through the application of genomic sequencing, healthcare professionals can detect these disorders early, potentially leading to improved outcomes and reduced risks for newborns. As we embrace this approach, it is essential to navigate the ethical considerations and support systems needed to empower patients and their families.